Cow's Milk Protein Allergy management
KEY MILESTONES
Successful management of cow’s milk protein allergy (CMPA) starts with an early diagnosis and requires ongoing support to ensure that infants and young children receive an appropriate elimination diet in order to reach their full potential. Nestlé Health Science is committed to helping you and your patients throughout the diagnosis and management journey.
1 - Starting the elimination diet
and food challenge

2 - Advise caregivers for
complementary feeding

3 - Monitor long-term growth
and development

4 - Periodically test for
tolerance
BREAST MILK IS THE GOLD STANDARD
FOR INFANTS WITH CMPA
Mothers of infants with CMPA should be supported to continue breastfeeding. Breast milk contains all the essential nutrients infants need in their first 6 months of life and should thereafter be complemented with a cow’s milk protein-free diet. In rare cases where infants react to cow’s milk transmitted through breast milk, mothers might have to eliminate cow’s milk proteins from their diet.
A clear improvement of CMPA symptoms is usually noticeable after the exclusion of cow’s milk protein in 2 to 4 weeks, and sometimes even earlier. It may be necessary for the mother to take daily calcium and vitamin D supplements while on a cow’s milk protein-free diet.1-3
To confirm or exclude the diagnosis, a controlled oral food challenge under medical supervision may be required.2 Learn more about food challenge here.
BREAST MILK NURTURE INFANTS' IMMUNE SYSTEMS
Infants with CMPA are at an increased risk of infections and future allergies.4-6 As breastfeeding has been shown to reduce the incidence of infections and future allergies, this provides yet another important reason to support mothers to breastfeed.7-11
These outcomes are attributed to diverse bioactive components present in breast milk, including human milk oligosaccharides (HMO).12 HMO are the third most abundant solid component of breast milk, and play an important immune-nurturing role.12
While there are over 200 of these structurally complex carbohydrates,12 two of them, 2’ Fucosyllactose (2’FL) and Lacto-N-(neo)tetraose (LNnT), account for more than 30% of HMO in breast milk.13
Several clinical studies reported the protective effect of breastfeeding
for infants, including a reduced incidence of:
Gastroenteritis and diarrhea 8,11
Respiratory tract infections 8,11
Atopic manifestations 7,9,10
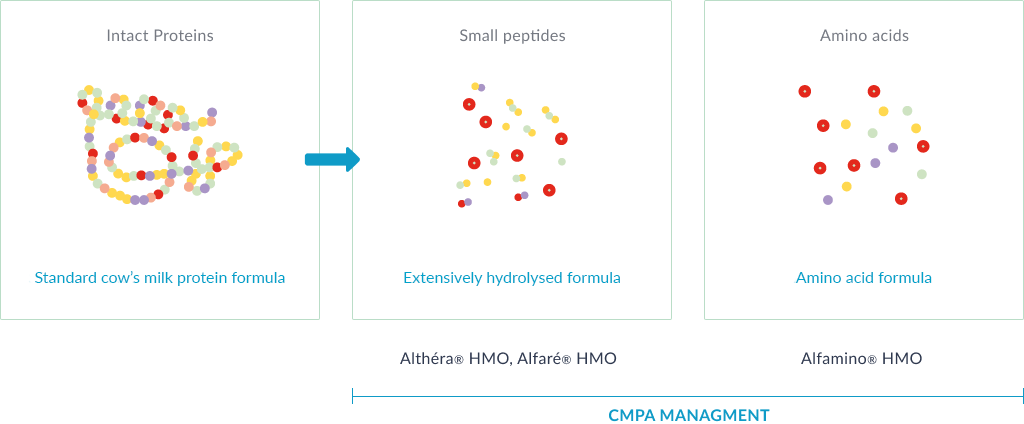
SPECIALTY FORMULAS FOR CMPA
When exclusive breastfeeding is not feasible, specialty formulas clinically proven to be hypoallergenic for infants with CMPA are recommended.1-3,14 These formulas contain all the necessary nutrients to support growth and development.
These specialty formulas can be:
Extensively hydrolysed formulas (eHFs): prepared from cow’s milk protein which have been hydrolysed (amongst other processes) to break them down into peptides, so that they are hypoallergenic and are less likely to cause an allergic reaction. eHFs, like Althéra® HMO and Alfaré® HMO, are recommended for first-line management of infants with CMPA.1-3,14
Amino acid-based formulas (AAFs): prepared from free amino acids. AAFs, such as Alfamino® HMO, are recommended in infants with severe symptoms of CMPA and/or multiple food allergies.1-3,14
Once an infant has eliminated cow’s milk protein from their diet with a specialty formula, CMPA symptoms typically resolve between 1-4 weeks, and sometimes sooner.2 To confirm or exclude the diagnosis, a controlled oral food challenge under medical supervision is often required. Learn more about food challenge here.
EXPERT CORNER: CMPA MANAGEMENT
In these videos, Professor Christophe Dupont provides an overview of CMPA and how to manage it effectively.
COMPLEMENTARY FEEDING AND CMPA
In the first six months of an infant’s life, exclusive breastfeeding is the preferred choice. In case breastfeeding is not possible for any reason, a special hypoallergenic formula for CMPA is recommended. Thereafter, it is time to introduce solid foods, as nutrient requirements increase.1-3,14
In infants with CMPA, whilst it is important to continue avoiding cow’s milk, other foods can be introduced just as it would be done with a non-allergic infant. There is no evidence that delaying the introduction of other potentially allergenic foods (e.g. wheat, soya, egg, fish, nuts…) will prevent the development of other food allergies. In fact, evidence is building that early rather than delayed introduction of these foods could be beneficial.15
A variety of different foods and flavours should be introduced into the weaning diet while still avoiding cow’s milk protein. During this time, specialty formula should still contribute a major part of an infant diet but it can also be used in recipes.
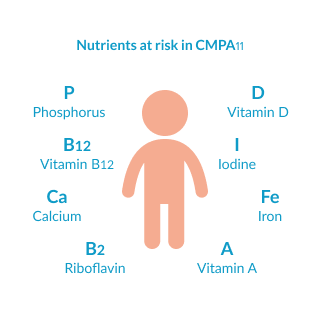
MONITORING LONG-TERM GROWTH IS ESSENTIALS
Elimination diets are necessary to prevent symptoms. However, they do increase the risk of nutritional deficiencies. In fact, several studies show how CMPA is linked to significantly lower growth in childhood if caregivers do not have professional dietetic support. It is therefore essential that caregivers are supported appropriately during this time. Nutrients at risk include calcium, vitamin D and iodine amongst others.16
WHEN AND HOW TO TEST FOR TOLERANCE
Half of all children with CMPA will outgrow it by 1-2 years of age, whilst the majority will outgrow it by 3 years of age, but it is difficult to predict when it will be achieved in each case.3,17 Non-IgE-mediated allergies tend to resolve more rapidly than IgE-mediated allergy or those with multiple food allergies.3
It is recommended to re-challenge children with CMPA every 6 to 12 months to assess whether they have developed tolerance to cow’s milk protein. Overly long dietary eliminations should be avoided as they might impair the quality of life of both the child and family, or increase the risk of impacting the child’s growth.2,3,14
Some guidelines recommend to start re-introduction with small amounts of milk in baked form (e.g. biscuits, cookies), as baking destroys a majority of epitopes causing the allergy. If the infant tolerates baked products well, introduction of products containing a larger amount of milk and/or in a less denatured form can be attempted.3 However, the practice differs between countries, and local recommendations about when and how to test for tolerance should be used.
Re-introduction may provoke allergic reactions and reappearance of symptoms. It should only be attempted with the guidance and under the supervision of a healthcare professional, as well as following local guidelines.
REAL-LIFE CASE STUDIES OF INFANTS WITH CMPA
Every infant is individual and the diversity of CMPA symptoms can make diagnosing and managing the condition particularly challenging. Here you will find several real-life case studies of infants with CMPA whose conditions have been successfully managed.

Daniel, 1 months old
Constipation and inconsolable crying

Joey, 4 months old
Severe eczema particularly on the face

Harry, 5 months old
Colic and immediate
gastrointestinal symptoms after feeding

Oliver, 2 weeks old
Constipation and unsettled

Vivian, 6 months old
Pale, lethargic, and dehydrated
with a weak cry
Emily, 7 months old
Symptoms of eczema and reflux
DANIEL WAS DIAGNOSED WITH IGE-MEDIATED CMPA AT 2 MONTHS OF AGE
Daniel is only two months old but he has been suffering from constipation and has been crying excessively for weeks. His parents could not understand why he was always distressed. "We haven't slept for nights and we cannot rest during the day because he cries constantly. We are really worried and don't know what it could be" said Daniel's parents.
When Daniel was one month old, he was hospitalised but the symptoms were not linked to CMPA and his parents were advised to try a partially hydrolysed infant formula for his constipation.
Unfortunately, there was no symptom relief and an upper gastrointestinal examination was performed. This revealed a high count of eosinophils in the blood. In addition, total IgE and cow's milk IgE were also high, which led to Daniel's diagnosis of CMPA. Daniel's parents were given Althéra®, an extensively hydrolysed formula (eHF) to manage her CMPA and asked to return to see the doctor in two weeks.
Within just two days of taking Althéra®, Daniel's constipation and crying had stopped! "We couldn't believe it! Daniel has never been happier...and we were so relieved that he was no longer suffering. Now we can all get a good night's sleep!" said Daniel's mother. Daniel's parents were pleased to return to the doctor two weeks later to tell him the good news!
Please note: These case studies are taken from medical reports from respective countries. Only the names of the patients and their families may have been changed.
EMILY WAS DIAGNSOSED WITH CMPA AT 10 MONTHS OF AGE
Emily was seven months old when she presented at a scheduled paediatric dietician appointment with resistant atopic dermatitis (eczema) and concomitant gastric-oesophageal reflux, for which she was on anti-reflux medication. Emily's weight was 6.3 kg and she was on the 9th percentile. A family history of atopic allergy was identified, as well as a zinc deficiency and skin infections for which zinc supplements and antibiotics had been prescribed. Emily was being breast fed by her mother, Abigail, who had tried eliminating wheat and dairy from her diet, as Emily's older sibling had a wheat allergy.
Abigal was advised to adhere to a strict cow's milk protein-free diet and asked to take calcium and vitamin D supplements. Emily's anti reflux medications were increased and she was given zinc supplements. Abigail carried on breast feeding and was advised to continue cow's milk protein elimination throughout the complementary feeding period.
Three months later, Emily re-presented with severe discoid eczema and food associated enterocolitis. At which point she was diagnosed with severe non-IgE-mediated food allergy. Her weight had not increased significantly and she was now faltering in growth with both zinc and vitamin D deficiency; Abigail was still breast feeding Emily and avoiding wheat, dairy, nuts and eggs but Emily was having episodes of loose stools. Emily was also not sleeping well due to itchiness and was admitted to the ward directly. It was upsetting for Abigail too "I've tried everything I can to help Emily but her symptoms seem to be getting worse I feel like a terrible mother."
Emily's symptoms were so severe that she was started on an amino acid-based formula, Alfamino®, via a nasogastric tube and after 24 hours bottle feeding was started. Within three days Emily was sleeping better and the eczema on her face and body was beginning to settle. She was discharged from hospital with zinc and vitamin D supplements and Alfamino®.
Emily's condition was reviewed after one month; she had gained 1.2 kg in weight and the eczema continued to improve considerably with less itchiness, redness and inflammation. Abigail noticed she was also sleeping better and the reflux had resolved, however she still had bouts of diarrhoea. " I am so happy that she is getting better - each day there is an improvement; the whole family can see it." Emily continued on Alfamino® and with complementary feeding in progress, Abigail was starting to introduce low atopic risk food.
Note: These case studies are taken from medical reports from respective countries. Only the names of the patients and their families may have been changed.
HARRY WAS DIAGNOSED WITH CMPA AT 5 MONTHS OF AGE
Harry was five months old when his paediatrician first referred him to a dietician for nutritional treatment of his persistent gastrointestinal problems. Harry had been suffering with what his paediatrician thought was gastro-oesophageal reflux (GOR) for some time and had undergone multiple treatments for this problem with no success. He was firstly treated with infant Gaviscon (alginate) but there was no improvement. He was prescribed Ranitidine (a H2 antagonist) and a pre-thickened formula, but these also failed.
When Harry first saw the dietician, an allergy focused clinical history was conducted in order to distinguish between IgE and non-IgE symptoms. He had colic type symptoms (unsettled, back arching and persistent crying) as well as both immediate and delayed GI symptoms (loose watery stools, wind, vomiting after each feed). Based on the mix of non-IgE and IgE-mediated symptoms, a serum specific IgE test was requested. Finally, a diagnosis of Cow's Milk Protein Allergy was made and Harry was started on an extensively hydrolysed infant specialty formula. Although there was some marginal improvement, Harry was still unsettled; his symptoms did not fully resolve and he continued to suffer from loose stools and frequent vomiting. After four weeks, Harry was prescribed an amino acid-based specialty infant formula, Alfamino®.
One week later, a telephone follow up was conducted with Harry's mother. She reported that Harry was doing much better on Alfamino®. "His stools are now soft and formed and his vomiting has significantly reduced. Overall he is much more settled:' A follow up in the clinic one month later revealed that all of Harry's symptoms had completely resolved thanks to Alfamino® and he was now fully weaned onto a cow's milk protein-free diet.
A few weeks later, Harry had an accidental exposure to baked cow's milk from a breadstick. This led to explosive diarrhoea within 30 minutes to 1 hour after consumption. The date and the location of a future food challenge is currently being discussed. Oral food challenges can be performed either at home or in a hospital. It can be safer to challenge those with immediate type reactions (usually IgE-mediated) in a hospital, depending on the severity of their initial symptoms. The results of the initial and repeated measurement of serum specific IgE will help doctors to make this decision.
Note: These case studies are taken from medical reports from respective countries. Only the names of the patients and their families may have been changed.
JOEY WAS DIAGNOSED WITH CMPA AT 12 MONTHS OF AGE
Joey was four months old when he had his first consultation. He was exclusively breastfed and he was suffering from severe atopic dermatitis which was especially prominent on his face. "We took Joey to see the doctor because he had a terrible rash on his face which he could not stop scratching. He was also not sleeping at night, which left us all sleep deprived" said his mother Agnes. There was a family history of allergic atopy; Joey's mother had atopic dermatitis as a child and still has an egg allergy. Joey's father also suffers from allergic rhinoconjunctivitis.
"Joey's doctor gave us a lot of information about atopic dermatitis which was very helpful:' Joey was given a basic skin treatment and a topical preparation containing cortisone. This led to an improvement of Joey's skin condition and a slight stabilisation. When Joey's parents began complementary feeding his skin deteriorated significantly. Joey's parents took him to see the doctor again and a food allergy test was performed, showing that Joey had a sensitisation to cow's milk protein and walnut. Joey's skin prick test also confirmed a sensitisation to cow's milk protein. Based on these results, Joey was prescribed Alfamino® as a milk substitute and his mother Agnes, who was still partially breastfeeding began a cow's milk protein-free diet. This resulted in a rapid healing of the skin.
After his 1st birthday, Joey was invited for a food challenge by his doctor. This resulted in an increase of the eczema, accompanied by acute urticaria. Alfamino® was therefore prescribed again as a cow's milk substitute, leaving Joey free of symptoms.
When Joey was two years old he began to eat processed milk products without any allergic symptoms. Joey's parents were so happy that Joey no longer had allergic symptoms and even happier that they could all get a good night's sleep. These case studies are taken from medical reports from respective countries.
Note: These case studies are taken from medical reports from respective countries. Only the names of the patients and their families may have been changed.
OLIVER WAS DIAGNOSED WITH CMPA AT 15 WEEKS OF AGE
Oliver was referred to a dietician at 11 weeks of age with a history of constipation, unsettledness and reflux without vomiting. Oliver initially presented with these symptoms at around two weeks old and was seen by a paediatrician as an outpatient.
Oliver was currently on a standard formula and had previously been prescribed lactulose to help with his constipation. His weight was on the 50th percentile however his height could not be measured due to his distress.
An allergy focused history was taken. With a certain incidence of asthma in the family and a suspicion of non-IgE-mediated symptoms, an elimination diet was considered, with the exclusion of cow's milk protein for two to eight weeks. The theory being that if symptoms do not improve then Cow's Milk Protein Allergy is unlikely.
Three sample tins of the lactose containing, extensively hydrolysed formula (eH F), Althéra® were prescribed and Oliver's parents were asked to contact the dietician if they felt that any improvement was seen so that a prescription could be arranged.
After six days, Oliver's parents phoned to say that Oliver was straining less to pass stools and was noticeably more settled. At the next appointment at 15 weeks (four weeks later), Oliver's weight was on the 75th - 91st percentile and his height on the 50th percentile.
Oliver's parents were really happy with his improvement; stools were being passed with ease and he was much happier overall. "Things are getting a lot easier and we are all less tense. It's so good to see him on form." Althéra® was well tolerated by Oliver and his weight had increased, although his intake was just under the recommended amount.
Oliver remained on Althéra® and his parents were given guidance on cow's milk protein-free complementary feeding and suitable first foods.
Note: These case studies are taken from medical reports from respective countries. Only the names of the patients and their families may have been changed.
VIVIAN WAS DIAGNOSED NON-IGE-MEDIATED FOOD PROTEIN INDUCED ENTEROCOLITIS SYNDROME (FPIES) AT 6 MONTHS OF AGE
Vivian was five months old when she was first given a cow's milk-based formula. "Vivian vomited more than four times two hours after feeding! We were so worried that we took her to the hospital straight away" said Vivian's parents. When the doctor first saw Vivian he reported that she looked lethargic, dehydrated and pale. She also cried weakly. Vivian was admitted immediately and put on an intravenous drip overnight. The doctors also decided to start Vivian on a course of intravenous antibiotics to treat any possible infection.
Vivian was referred to an allergist to investigate her condition further. She was tested for Cow's Milk Protein Allergy with a skin prick-test and a blood test but she tested negative for Cow's Milk Protein Allergy with both tests. Vivian was then diagnosed with a non-IgE-mediated Cow's Milk Protein Allergy called food protein-induced enterocolitis syndrome (FPIES).
The allergist offered Vivian's parents an extensively hydrolysed specialty formula, Alfaré® to help manage her Cow's Milk Protein Allergy. Vivian tolerated Alfaré® well, was successfully weaned over to Alfaré® and also started with cow's milk protein-free complementary feeding. Her parents were advised to adhere to strict avoidance of cow's milk protein. They were also advised to read food labels carefully to ensure complete avoidance of dairy products until a formal food challenge could be conducted. "At first we were really nervous to start giving Vivian complementary solid foods because we were told that there was a small risk of FPI ES to grains, meats, fruits and vegetables, but the dietician gave us lots of helpful advice so we had no problems introducing Vivian to lots of different baby foods" said Vivian's father RahuI.
When Vivian was seven months old, she was accidently given some yoghurt melts to eat at a birthday party. About two hours later, Vivian began vomiting, but this time it was less severe than before.
At 24 months old, Vivian was given a formal cow's milk challenge as an inpatient at hospital. Senali, Vivian's mother couldn't stop smiling "We were so happy that she didn't react to the cow's milk and even happier that her FPIES had resolved!"
Note: These case studies are taken from medical reports from respective countries. Only the names of the patients and their families may have been changed.
OUR RANGE OF TAILOR-MADE NUTRITIONAL SOLUTIONS
Nestlé Health Science has a range of nutritional solutions that are tailor-made to meet the specific needs of infants with CMPA. Our formulas are nutritionally complete to support normal growth and development in infants, with the addition of HMO* to support growing immune systems.
ADDITIONAL RESOURCES
VISIT OUR RESOURCE CENTRE
* Structurally identical Human Milk Oligosaccharides (HMO) are not sourced from human milk
REFERENCES
- Koletzko S, et al. Diagnostic Approach and Management of Cow’s-Milk Protein Allergy in Infants and Children: ESPGHAN GI Committee Practical Guidelines. J Pediatr Gastroenterol Nutr 2012;55(2):221-229.
- Prescott SL, et al. A global survey on changing patterns of food allergy burden in children. World Allergy Organ J. 2013;6(1) :21
- Cekola P, et al. Clinical use and safety of an amino acid-based infant formula in a real world setting. Abstract presented at NASPGHAN. Chicago, IL, USA, October 2019.
- Høst A. Cow’s milk protein allergy and intolerance in infancy. Some clinical, epidemiological and immunological aspects. Pediatr Allergy Immunol. 1994;5:1-36.
- Jalonen T. Identical intestinal permeability changes in children with different clinical manifestations of cow’s milk allergy. J allergy Clin Immunol 1991;88(5):737-742.
- Crittenden RG and Bennett LE. Cow’s Milk Allergy: A Complex Disorder. J Am Coll Nutr 2005;24(6suppl):582S–591S.
- Maslin K, et al. Palatability of hypoallergenic formulas for cow’s milk allergy and healthcare professional recommendation. Pediatric Allergy and Immunol. 2018; 29:857-862.
- Francavilla R, et al. Effect of lactose on gut microbiota and metabolome of infants with cow’s milk allergy. Pediatr Allergy Immunol. 2012;23:420-427.
- Abrams SA, et al. Calcium and zinc absorption from lactose-containing and lactose-free infant formulas. Am J Clin Nutr. 2002;76(2):442-6.
- Petrus NCM, et al. Remaining symptoms in half the children treated for milk allergy. Eur J Pediatr. 2015; 174:759-765.
- Chauveau, A, et al. Immediate hypersensitivity to extensively hydrolysed formulas: An important reminder. Pediatric Allergy and Immunology. 2016;27(5):541-543.
- Nutten S, et al. Peptide size profile and residual immunogenic milk protein or peptide content in extensively hydrolysed infant formulas. Allergy. 2019
- Nowak-Wegrzyn A, et al. Confirmed Hypoallergenicity of a Novel Whey-Based Extensively Hydrolyzed Infant Formula Containing Two Human Milk Oligosaccharides. Nutrients. 2019;11(7):E1447.
- Nowak-Wegrzyn A, et al. Hypoallergenicity of a whey-based, extensively hydrolysed infant formula prepared with nonporcine enzymes. Allergy. 2019;74(8):1582-1584.
- Niggemann, B, et al. Safety and efficacy of a new extensively hydrolysed formula for infants with cow’s milk protein allergy. Pediatr Allergy Immunol. 2008. 19(4):348-54.
- Vandenplas Y, et al. A workshop report on the development of the Cow’s Milk-related Symptom Score awareness tool for young children. Acta Paediatr. 2015;104(4):334-339.
- Vandenplas Y, et al. Pooled analysis of the Cow’s Milk-related Symptom Score (CoMiSSTM) as a predictor for cow’s milk related symptoms. Pediatr Gastroenterol Hepatol Nutr. 2017;20(1):22-26.
- Vandenplas Y, et al. The Cow Milk Symptom Score (CoMiSSTM) in presumed healthy infants. PLoS One. 2018;13(7):e0200603.
- Nestlé Health Science, data on file. CINNAMON study.



